Saying Goodbye To The Kojo Nnamdi Show
On this last episode, we look back on 23 years of joyous, difficult and always informative conversation.
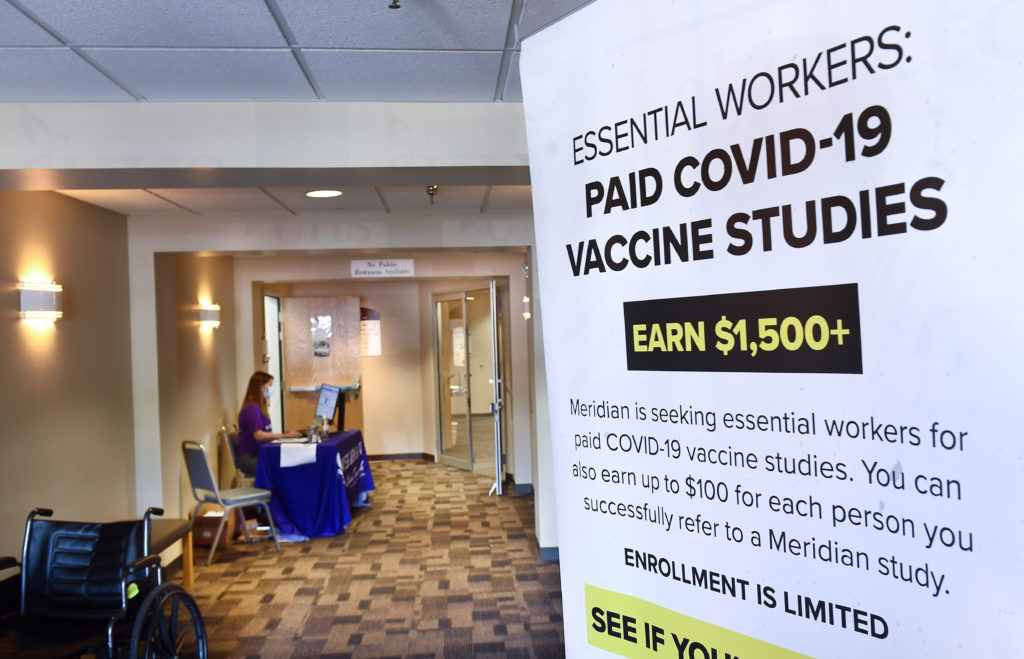
A poster is displayed in the entrance way looking for volunteers as the world's biggest study of a possible COVID-19 vaccine, developed by the National Institutes of Health and Moderna Inc., gets underway in late July.
As we enter month six of the pandemic, there are now nearly 30 million COVID-19 cases worldwide — and close to one million deaths.
In ordinary times, it takes years of research and testing to develop an effective vaccine. But in a pandemic, it’s “Operation Warp Speed.” U.S. researchers set an ambitious goal at the start of the year: to develop a coronavirus vaccine within 12 to 18 months.
With seven vaccines now in the final stages of clinical trial, including one at George Washington University, how much progress has been made? How hopeful — or skeptical — should we be? And how soon can we expect a safe and effective vaccine for all?
In times of uncertainty, we look to medical professionals for guidance. The clinical director of GW’s vaccine research unit Dr. David Diemert and public health expert Dr. Leana Wen join us to share their expertise and answer your essential questions.
Produced by Julie Depenbrock
KOJO NNAMDIYou're tuned in to The Kojo Nnamdi Show on WAMU 88.5, welcome. As we enter month six of the pandemic there are now nearly 30 million COVID cases worldwide and close to one million deaths. In ordinary times it takes years of research and testing to develop an effective vaccine, but as we know these are no ordinary times. Researches and private companies all over the world are trying to develop a coronavirus vaccine in record time dubbed "Operation Warp Speed." The NIH has seven vaccines in various stages of clinical trial inducing one at George Washington University.
KOJO NNAMDISo how soon can we expect a safe and effective vaccine for all? Joining us to discuss this is Dr. David Diemert. He's a professor at George Washington University School of Medicine and Health Sciences and the Clinical Director of the GW vaccine research unit. Dr. Diemert, thank you for joining us. Also joining us is Dr. Leana Wen, an Emergency Physician, a Contributing Columnist for the Washington Post and a Visiting Professor At George Washington University. She formerly served as Baltimore's Health Commissioner. Dr. Wen, thank you for joining us. Good to talk to you again.
DR. LEANA WENNice to talk to you, Kojo. Thank you.
NNAMDIDr. Wen, how many vaccine trials currently taking place around the world and are any showing promise?
WENSo there are dozens and dozens of potential vaccine candidates around the world. There are nine vaccines that are in this critical phase three trial, which is really important, because this is the population based level. This is when a vaccine is injected into people. A placebo is also injected into large numbers of people. And we then compare. We then compare to make sure that the vaccine actually is protective for these individuals from getting COVID-19.
WENAnd the safety issue is also when this is -- when the rubber really meets the road, because sometimes there may be rare effects that you'll only see when you test it in tens of thousands of individuals. And there is certainly a lot of promise, but I know that we'll be discussing more about this. The importance of not valuing speed as the only metric that making sure we have a vaccine that's safe, making sure that it's effective is going to be so critical because the last thing that we want is to further erode trust in vaccines and indeed in science if we end up releasing a vaccine candidate too soon.
NNAMDIDr. Diemert, tell us about the vaccine trial you're leading at George Washington University. What stage are you at and how is it progressing?
DR. DAVID DIEMERTThanks, Kojo. So we are one of the sites for the first phase three trial to occur in the United States. And that's the Moderna NIH phase three trial of the COVID vaccine. So we are about four and a half weeks into enrolling at our site here in GW. The study as a whole started -- the first person was vaccinated on July the 27th. And as a whole nationwide, at about 100 different sites that are enrolling, we're up to about 25,000 people enrolled out of 30,000. That's the goal.
NNAMDIWhat is your specific role as GW's clinical director of vaccine research?
DIEMERTSo I am what's called the principal investigator at our site for the study. And that basically means that I'm the physician who's kind of in charge of everything that happens and in particular I'm responsible for the safety of the people that were enrolling into the trial at our site here.
NNAMDIWhat more can you tell us about this potential vaccine?
WENSo it's what's called an MRNA or a messenger RNA vaccine. It's a relatively new type of vaccine that really consists of a little piece of genetic code that kind of tricks the body into making a protein that's normally found on the surface of the virus. And the whole point of that is to kind of force the person who gets the vaccine, force their immune system to develop antibodies against that particular protein so that in the future if someone is exposed to the virus, you know, transmitting in the community that they would be protected. So that's kind of the concept.
NNAMDIDr. Wen, ordinarily the development of a vaccine takes years. In the past, vaccines taken from the pretty clinical phase required an average of almost 11 years and had a six percent probability of making it to the market. So what's different this time around?
WENWell, we are in the middle of the worst public health catastrophe that we have seen in a lifetime. And there are efforts all around the world. I mean, scientists are working all around the world. We're expediting this and investing in the development of this vaccine. And so I think this is why there is so much hope that when we have this many shots on goal if you will, the hope is that one or ideally more than one candidate will be found to be safe and effective. But I do think that getting our -- holding our expectations in check is going to be important.
WENOne is what you said, Kojo, that the fastest that a vaccine has been developed in the past was four years, and so if we get a vaccine within a year that's going to be in record time. And while we do want to do our best to expedite the development of a vaccine, we all want a vaccine to be out there as fast as we can, we cannot compromise safety, because we are giving this vaccine to millions of otherwise healthy people. So we cannot compromise safety and we certainly cannot remove our standards when it comes to -- or lower our standards when it comes to efficacy, because we don't want to give people the false reassurance that what they're taking will protect them from COVID-19 when it doesn't.
WENAnd I think setting the expectation too that the vaccine is not a silver bullet that first of all it's going to take a long time. Even after approval getting hundreds of millions of doses out to people is going to take many months. Very likely this will also require two doses of the vaccine. That's complicating things. And you'll also then will need to sets of these. You'll need to have the vials and the syringes and you have to have all these other methods to get the vaccine out to people. And even then it may well be that this vaccine is not anywhere close to 100 percent effective. It may be at best 70 to 75 percent effective, which means that we will still be maintaining some level of our public health hygiene methods.
WENSome measure of handwashing, wearing masks and social distancing will continue for the foreseeable future. So I think that expectation needs to be set that it's not as if a vaccine -- even if it's approved let's say by January that it's not as if life is going to return back to prepandemic normal immediately it will take many months if not years for that to occur.
NNAMDIWell, Dr. Wen, President Trump is promising a vaccine in record time saying it could even come sometime in October. Is that a real possibility?
WENLook, I just don't understand how that's literally going to occur. Many of these vaccine trials, they're still in the middle of recruiting candidates -- recruiting participants. And they will need to receive two doses of the vaccine spaced several weeks apart. And then it takes time to develop antibodies. And then it takes further time for people to be exposed to COVID-19 so that we can compare the placebo arm to the arm that actually received the vaccine. And so October is next month. I just don't see how we're going to get any kind of meaningful results from these studies by end of October. And I think that putting a date certain and using that as the metric is inherently dangerous, because we really should not be valuing speed over everything else.
NNAMDIHere now is Dr. Mize in Upstate Michigan. Dr. Mize, you're on the air. Go ahead, please.
DR. MIZEYeah, Dr. Mize, COVID doctor up here at the Sault Saint Marie Tribe up in Upstate Michigan. And we had just gotten the underground word that we would be getting prepared to get the vaccine I think at the end of November. And needlessness to say looking at the historical treatment of Native Americans the population here is not too crazy about this idea getting the feeling they may end up being the Guinea pigs for this vaccine before it's unleashed on the rest of the country.
NNAMDICare to comment on that, Dr. Wen.
WENI mean, I completely understand and can see exactly what Dr. Mize is saying. There are many communities around the country, Native American populations, African American populations and many others that have reason to distrust based on actually recent histories of discrimination and of being used as test subjects, and this is why that trust in this vaccine is going to be so important, because there is already existing skepticism, some for very good reasons.
WENWe need to make sure that whatever vaccine is approved follows the strict scientific standards that no shortcuts are taken that we're not moving the goalpost that it is not political ideology or partisanship that's driving approval of the vaccine. And there needs to be far more concerted efforts to reach out to communities like the one that Dr. Mize is serving to do public education. But that public education has to follow the fact that approval of this vaccine and distribution should be equitable and it should certainly not be before all the science is there to prove that it's safe and effective.
NNAMDIDr. Mize, thank you for your call. Dr. Diemert, what's being done to speed up the process for the COVID vaccine and what are the potential risks?
DIEMERTThanks for that question, Kojo. So I would actually answer that by saying we are not doing anything to speed up at least this particular trial. The only thing that maybe is being done in a more rapid fashion than like a routine phase three trial is the pace of enrollment. So we're just enrolling a lot more people in a shorter period of time than would otherwise happen in a phase three trial. But for an individual participant, who gets enrolled into the trial there's no speeding up. We're still doing the same number of follow-up visits, the same timeframe. Each person is going to get followed for two years. They get two doses of vaccine a month apart. That is not being compressed.
DIEMERTWhat has been compressed definitely is the pace of enrollment. And they've done that by having a lot more sites around the country than they otherwise would. So we're able to enroll more people in a shorter period of time. But for this trial itself, I would not say it's being sped up. Definitely the clinical development as a whole is being compressed. And they've done that by staggering the phase one and phase two and phase three trials. But now that we're at the phase three phase it's being done in the manner -- the scientifically valid manner than it should.
NNAMDIGoing to take a short break and then return to this conversation about coronavirus vaccines. I'm Kojo Nnamdi.
NNAMDIWelcome back. We've been exploring the possibility, probability and likelihood of a coronavirus vaccine with Dr. Leana Wen, an Emergency Physician, Contributing Columnist for the Washington City Post and a Visiting Professor At George Washington University. And Dr. David Diemert, a professor at George Washington University School of Medicine and Health Sciences and the Clinical Director of the GW vaccine research unit. Dr. Diemert, what can you tell us about those who have qualified for the trial at George Washington?
DIEMERTSo we've already enrolled about 230 participants at our site. We're now starting to get into the second dose of vaccine, because it's a two dose schedule. So each participant gets a dose of vaccine a month apart. So we started enrolling about a month. We're starting with the second vaccinations. But we're still enrolling people. And probably we'll have another couple of weeks.
NNAMDII think we may have temporarily lost Dr. Diemert. Here is Vicky in West Virginia. Vicky, you're on the air. Go ahead, please.
VICKYComment that I've been working in healthcare going on 40 years. I'm definitely pro-vaccine. And I'm currently working on my graduate degree in epidemiology. But I'm not willing to take anything that -- any vaccine that hasn't been tested maybe one to two years. I agree that if something comes out and it doesn't work, the public is just going to lose more trust. I would rather just take the regular flu vaccine to help build my immune function and try to prevent from getting in the COVID-19.
NNAMDISo you're saying, Vicky, that you would not take a COVID-19 vaccine under any circumstances?
VICKYNot until it's been out for one to two years.
NNAMDIOkay.
VICKYI just feel it's being rushed for political reasons at this point. And -- I mean, at least part of it is being rushed for political reasons. And I just would be more comfortable waiting at least a year for myself. And for those who want to take it, I don't criticize them at all.
NNAMDIOkay. We'll address the issue of the politics of this shortly in this discussion. But when we left Dr. Diemert -- Dr. Diemert you were explaining to us about those who've qualified for the trial at George Washington.
DIEMERTRight. Sorry. So we have enrolled 250 study participants -- so far of almost 250 participants at our site. And we've been enrolling now for about a month. So we're now getting into the second dose of vaccine for the people who were initially enrolled a month ago. But we're continuing to enroll new study participants. And probably we'll have another couple of weeks to complete enrollment at our site before the overall 30,000 participant number is reached countrywide for the study.
NNAMDIHere's Marlene in Silver Spring, Maryland. Marlene, you're on the air. Go ahead please.
MARLENEThank you for taking my call. So I was curious, because I volunteered now twice for the selection process. Understood that you needed African Americans for the vaccine and so I went ahead and volunteered. I got no response at all. And I was wondering about the qualifying questions. And is there a way that you can tell us whether or not -- which questions are disqualifying. I guess you can't say that on air. But is it possible to notify those that they will not be selected so we can stop volunteering?
NNAMDIDr. Diemert, how can people who are interested in volunteering sign up for your consideration? And the question that Marlene is asking is exactly what is taken into consideration to decide whether a volunteer can or cannot participate?
DIEMERTSure. So I can answer that question about who is eligible. So basically anyone over the age of 18 can be eligible as long as they're not pregnant or breastfeeding or have a condition that would cause your immune system not to work well. Like someone say who is taking medication for an organ transplant. Also if you've had COVID already you're not eligible. But pretty much anyone else can participate in the study. Now, in terms of volunteering at our site there are two main methods that people have been kind of signing up on the registries. There's a national registry that's run by the NIH. And that registry has had over 500,000 people join. So it's just been an overwhelming number of people. We can get people through that registry. But it's just so many people that it's hard for us to contact everyone. So that might be one of the issues with Marlene.
DIEMERTSo much better for getting in touch with our site and for us being able to reach to you would be going to our website, which is the GW Vaccine Research Unit. You can just Google it and complete -- we have a mini survey that's secure that you can sign up that way or call 202-994-0047 or email us at covid19vaxtrial@gwu.edu. That's covid19vax -- v-a-x-t-r-i-a-l.
NNAMDIAnd Dr. Diemert, can you repeat the phone number, please.
DIEMERTSure, 202-994-0047.
NNAMDIMarlene, thank you for your call. Marie from Loudoun County called, but could not stay on the line. Marie's question is: After all of the volunteers have been vaccinated, what's the process for finding out if the vaccine is effective?
DIEMERTSure. So I can answer that. We will be monitoring all of our study participants for developing COVID. So positive, you know, nasal swap test plus symptoms. So that's the primary end point when you're talking about a phase three vaccine trial there's always a primary end point that's going to determine whether or not the vaccine works or not. So for this trial it's symptomatic COVID infection. So positive test for COVID and symptoms. So we're going to basically follow everyone for that. And then they'll compare the number of cases in those who got the placebo versus those who got the vaccine and that's how we're going to figure out whether or not the vaccine works and is effective.
NNAMDIDr. Wen, as we said, Black and Latino populations have been disproportionately affected by COVID-19 and they're inclusion in the vaccine trials has been a priority. But it's also important to be sensitive to the legacy of mistrust based on past and current medical mistreatment. How are physicians working to build trust with Black and Latino volunteers?
WENThis is such an important question, Kojo. And it does tie to what you just said, which is that we do know that black, Latino, Native Americans are disproportionately affected by COVID-19, and therefore must be included in the clinical trials as well. Trust cannot be built overnight. It needs to be established with the most trusted messengers, including enlisting the help of pastors and community leaders to assist in this process.
WENAnd people need to understand, too, what is in it for them to help in this process? Because, otherwise, I think these are the same communities that, given the legacies of discrimination and experimentation, feel like they may be the subjects for getting experimented on versus having something that is helping them in the community.
WENAnd, you know, this ties to, I think, Kojo, the question that Vicki had asked a while ago about trust in vaccines, overall. And, unfortunately, I am hearing from more and more people that if we do this the wrong way, if we end up releasing a vaccine without the proper safeguards in place, or even if the safeguards are in place, but there has been so much talk about pushing the timeline forward and having a political process drive the decision rather than a scientific rigor, if that narrative is out there, then it doesn't only hurt the trust in this vaccine. It may hurt the trust in other vaccines and in the scientific process, overall.
WENAnd so, I think, again, emphasizing that the process has to be based on scientific rigor and not on political expediency. It's so important. And just one more thing here too about what Vicki said about flu vaccines. I hope that everyone listening will see this as the opportunity to do what we can now, which includes everyone should get the flu vaccine. Every year, there are hundreds of thousands of hospitalizations because of the flu, tens of thousands of deaths from the flu.
WENWe don't yet have a vaccine to COVID-19, but we do have a vaccine to the flu, and so we should all do our part. Get the flu vaccine to protect ourselves and others. Now is the best time to be doing that, September and October, before October 31st. That's the best time for people to be getting the flu vaccine, so please get it now.
NNAMDIWell, Dr. Wen, you may have addressed this Tweet we have from Atusa, but you may want to reiterate it. Atusa tweets: Very concerning is the attitude of public, the level of skepticism toward safety and mixing signs in politics. I have been surprised hearing this from my colleagues, and they are hesitant to take the vaccine once available. What is being done to address this issue? You just mentioned it, but you might want to reiterate, politics.
WENThat's right, and much more, I think, needs to be done. So, there are some positive steps that have been taken. There are nine pharmaceutical CEOs who've taken the initiative themselves to say that they will not submit for approval until they are confident about their studies. We've also seen FDA career scientists who are not political appointees, but are career officials, come out and say that they will not approve something.
WENAnd, of course, Dr. Francis Collins, the head of the NIH, Dr. Anthony Fauci, they've all been trying to reassure the American people. And they are, I think, for many of us trusted messengers, trusted scientists in this regard. But I think the federal government can do even more. They can make sure that the data around vaccines are available for everyone so that scientists who are outside of the government can also have access to this data and look at the data ourselves.
WENThey can also ensure that the benchmarks are set in advance, so that we don't have the issue of a moving goalpost. And I think that President Trump and other elected officials really need to stop giving arbitrary deadlines in trying to tie vaccine approval to a timeline like elections. Because, by definition, that is political and partisan in nature and, I think, further seeds doubt, and may prevent people from getting the vaccine even if one that is safe and effective comes out.
NNAMDIDr. Diemert, in the minute or so we have left in this segment, many vaccine trials aren't reflecting the diversity we talked about earlier. I understand GW has met an ambitious goal and that half of your participants are black or Latino volunteers. What did it take to get there and how did you address the issues Dr. Wen mentioned?
DIEMERTYes, that's correct. It's a bit of a moving target, since we're still enrolling, but as of now, we have over 50 percent of our people, at our site at least, who are Latinx or African American. So, we did a lot of outreach in explaining the study in as many different forums that we could, so that we reached a broad segment of the population. So, there was, I think, taking advantage of the existing relationships that GW has, particularly through this whole public health with Dr. Manya Magnus, community advisory boards that were already in place for all of their great work around HIV prevention...
NNAMDIOkay.
DIEMERT...expanding that to really get the word out to the community.
NNAMDIGot to take a short break. When we come back, we'll continue this conversation, but you can still give us a call. Are you nervous about safety risks, given how fast a vaccine's being developed? I'm Kojo Nnamdi.
NNAMDIWelcome back to this conversation about coronavirus vaccines. Here is Martha in Alexandria, Virginia. Martha, you're on the air. Go ahead, please.
MARTHAYes, thank you, Kojo. I actually listened to the first, I think the last time was the first time a GW representative came and talked about the vaccine trial. And so, I signed up. And when I talked to friends and family, they said, what about the side effects? And so, I looked up -- actually I only looked at one article. It scared me so much that I called and canceled. So, what are -- what is -- in case I get the actual vaccine, what are possible side effects?
NNAMDIDr. Wen, side effects, safety risks. What has been reported so far with these vaccine trials?
WENWell, the vaccine trials in phase one and in phase two where they were testing in small numbers of people, so we're talking about dozens of people, there have been relatively mild side effects. So, certainly, there could be the site -- there could be a reaction at the site, so you could get inflammation at the site. Some people have experienced fever, muscle aches, joint aches, relatively mild symptoms that are self-contained. And therefore, it was deemed that the vaccine was safe to proceed to the next phase, which is phase three, injecting into large numbers of people to see if there are other types of side effects.
WENNow, there is a trial that was temporarily put on hold by the vaccine maker AstraZeneca, where it appears that a candidate, or a patient who is enrolled in the trial and received this candidate vaccine got a very serious reaction called Transverse Myelitis, which is inflammation of the spinal cord. It's still being investigated about what -- how and if the vaccine actually contributed to that reaction. But I think it is a sign that proper safeguards are being followed in this regard. And those types of reactions should be extremely rare and investigated thoroughly.
NNAMDIHere now is Michael in Washington, D.C. Michael, you're on the air. Go ahead, please.
MICHAELThank you. Thanks for the session. I had a question about the ethics of doing this and was going to be for Dr. Diemert, but maybe Dr. Wen can speak to it. I'm wondering, we already have seen these trials take place in Africa, Brazil, in the Third World. And my question was, to what extent are folks at GW relying on this data in forming their work? How do we square the, what you could call maybe, medical apartheid in where this testing is happening?
MICHAELAre folks disproportionately black and brown and poor in the GW work? How is this all adding up? These trials aren't happening in isolation, even though GW's got the relationship with Moderna. The folks communicate through the peer review literature, and so forth. How do you square the uneven nature of the testing around the globe and with different black and brown bodies? And I'll take my answer off the air.
NNAMDIWell, Dr. Wen, in addition to that, Paula from Arlington called, but couldn't stay on the line. She said, we've heard about the disproportionate effect on people of color. Are these tests, the ones in Africa or Latin America, to get a more accurate reading of how the vaccine affects these groups?
WENThese are really excellent questions. And I think the ethnics around both the vaccine testing and distribution are really important. Because the last thing that we would want to do, to the question -- very important point that was raised by Michael about this medical apartheid, the last thing that you would want to do is to do testing in a particular population and then not make the therapy available to those same populations.
WENAs in you would not want to be testing, let's say, in African Americans, Latino Americans, and then not prioritizing those same populations when the vaccine is out and only providing it to those who are privileged, who tend to be white and more advantaged in other ways. So, that distribution and the fairness and equity and distribution also has to be established in advance. And there are important frameworks in that regard.
WENThe National Academies, for example, has come out with a framework that talks about how, of course, those who are frontline workers, who are particularly vulnerable, older individuals, nursing home residents should be prioritized, but also black and brown people, as those who are disproportionately affected should also be prioritized when it comes to vaccines, too.
WENI think there is a separate question, though, about where the vaccine trials are being conducted because there is a practical consideration, too. So, as an example, there is a -- there are Chinese vaccine manufacturers that have to do their trials not in China. And it's not because they don’t' want to experiment on the Chinese population, but for a practical reason, which is that right now there isn't enough virus in China for this trial to be conducted. Which is not a problem that we have here in the U.S.
WENBecause, unfortunately, there is virus in so many parts of our country, viral surges in so many parts of the country. But we have to do the trials in a place where there is enough infection, because otherwise you cannot test whether the placebo group versus the group that got the vaccine is protected from getting the virus. And so, again, I think that there are very serious ethics considerations, including informed consent, but also the distribution of that vaccine is going to be really important, too.
NNAMDII think Dr. Diemert is back with us. Dr. Diemert, are you there?
DIEMERTI am here.
NNAMDIOkay. I think you were cut off while you were responding to a question.
DIEMERTWhich question was that?
NNAMDIThat's an excellent point. I think it had to do with the reported side effects with the Moderna trial.
DIEMERTYes. So, for the Moderna vaccine, most of the side effects really relate to what we call injection site reaction. So, some soreness, tenderness, a bit of swelling at the site where the vaccine was given. It usually starts the day after. Doesn't last for more than a day or two. Some people have some more general side effects, feeling tired, a bit of a headache, maybe some sore muscles for a day or so.
DIEMERTBut in all other people so far who have been vaccinated, even nationwide, 25,000, it hasn't been much more than that. There have been no serious side effects from the vaccine, at least the Moderna vaccine. I should qualify that saying that different vaccines can have different side effects, but at least with the Moderna vaccine, that's what we've been seeing.
NNAMDIHere's Michelle in Silver Spring, Maryland. Michelle, you're on the air. Go ahead, please.
MICHELLEHi. Thanks, Kojo. Great show, as usual. We know that viruses interact with each other and that vaccines can impact other viruses. Is there -- are there any studies being done to look at the impact of the flu shot on the novel coronavirus?
NNAMDIDr. Wen?
WENSo, I've received this question a lot from patients wondering if they should still be getting their other vaccines. And the answer is absolutely, yes. This is a different vaccine. There should not be effects on other types of vaccines. And, actually, what I'm really concerned about is how people have fallen behind in their preventive health screenings. We know that children, for example, have not been getting their routine childhood vaccinations, leading to concerns about resurgence of measles and resurgence of other diseases that actually are preventable through vaccines. So, please, get your routine vaccines and absolutely get the flu vaccine this year.
NNAMDIThank you very much for your call, Michelle. Dr. Wen, many independent scientists and public health officials are calling for greater transparency from drug companies involved in the vaccine race. What's going on, here? What are your thoughts about this?
WENWell, I think this has to do with this level of distrust that we have, that the American public has in our regulators. Because the role of the Food and Drug Administration, the FDA, is to be a regulator, is to protect us, it to look at all the science and data coming from these companies and to make an unbiased decision based on science.
WENAnd, unfortunately, because the FDA, the CDC and other institutions have lost a lot of trust and credibility, because it's been thought that they are subject to a lot of political pressure -- I mean, there are phenomenal scientists, don't get me wrong, working in these institutions. It's not them. It's that they're being subject to pressures from on top. And, as a result, another way to get more information is to have these companies themselves be more transparent about their data.
WENSo, I think that that can and should be done. Again, I think that having independent evaluation and having the data available to external bodies, external scientists and public health leaders, will be important, because these are people who are not beholden to the Trump administration. But I also don't think that we should let the FDA off the hook. It's still their job, and they still have to do their job to protect the American people.
NNAMDIDr. Diemert, we got an email from Bill in Fairfax, who asked: What makes it easier or harder to develop a vaccine for a given disease? For example, it seems like there's been amazing progress toward developing a COVID-19 vaccine, but for diseases like malaria or AIDs, vaccine development has been very slow. Dr. Diemert?
DIEMERTGreat question. It really depends on the organism that you're trying to develop a vaccine for. So, in general, it's much easier to develop a vaccine for viruses, just because they're much simpler organisms than, say, malaria, which is a parasite, much more complex. And the other thing is how rapidly the organism changes, you know, when it mutates and, you know, new strains arise. It's much more difficult to develop vaccines for organisms that do that, and malaria and HIV both fit into that category. We don't see the same level of -- at least not yet -- change over time and mutations in the coronavirus vaccine -- sorry, the COVID virus.
NNAMDIDr. Wen, we only have about 30 seconds left, but tell us, what is herd immunity and how many people have to be vaccinated to achieve herd immunity?
WENSo, the idea is that you need to have a certain percentage of a population to be infected or to have acquired immunity through the vaccine in order to protect everybody else. So, we're looking at at least 60 to 80 percent of the population. Herd immunity through vaccination is a good idea and something we should strive for.
WENThrough natural infection is extremely dangerous and does not work, because it means that we're looking at maybe 2 million people in the U.S. who would have to die before we could potentially even have herd immunity through just acquiring the infection. So, we should aim for the vaccine, but in the meantime, take every precaution when it comes to mask wearing, physical distancing and protecting ourselves.
NNAMDIDr. Leana Wen, Dr. David Diemert, thank you both for joining us. Today's show was produced by Julie Depenbrock. On an upcoming Kojo Show, we're remembering lives lost to COVID-19. Has someone close to you passed away from the coronavirus? Share your story with us. Go to kojoshow.org and click on the banner that says "Remembering the Lives Lost."
NNAMDIComing up tomorrow, we check in with Jason Wright, the Washington football team's new president and the NFL's first black president on his new role, the team's name change and this moment of racial reckoning. Plus, over the years, Black Lives Matter has expanded from fighting for justice and equality in policing to other areas, including the workplace where people of color are underrepresented in management and leadership. How are organizations addressing that issue? That all starts tomorrow, at noon. Until then, thank you for listening and stay safe. I'm Kojo Nnamdi.
On this last episode, we look back on 23 years of joyous, difficult and always informative conversation.
Kojo talks with author Briana Thomas about her book “Black Broadway In Washington D.C.,” and the District’s rich Black history.
Poet, essayist and editor Kevin Young is the second director of the Smithsonian's National Museum of African American History and Culture. He joins Kojo to talk about his vision for the museum and how it can help us make sense of this moment in history.
Ms. Woodruff joins us to talk about her successful career in broadcasting, how the field of journalism has changed over the decades and why she chose to make D.C. home.